Part 6_Essay Series, Title: The Last Companion, No Humanoid
Part 6_v02
Japan is aging faster than any other country. With a shrinking workforce and growing elder population, the challenge of providing quality elder care is urgent. While many have imagined humanoid robots as the solution, Japan's experience tells another story. This essay explores a more grounded vision: not robots with eyes and arms, but intelligent environments — specifically, the Symbiotic Bed.
This is a paid essay, available for a one-time payment of 10 EUR.
👉 [Click here to purchase and unlock the full text]
https://www.kindlman.blog/part-6_essay-series-title-the-last-companion-no-humanoid/
The Reality in Japan
Since 2012, Japan's Ministry of Economy, Trade and Industry (METI) and Ministry of Health, Labour and Welfare (MHLW) have promoted AI, robotics, and sensor technologies in elder care. Yet despite government support, humanoid robots like Robear rarely appear in nursing homes. Why? The reasons are both technical and human: safety risks, high cost, complexity, and the uncomfortable emotional response many feel toward human-like machines. Rather than helping, such designs often create fear or unrealistic expectations.
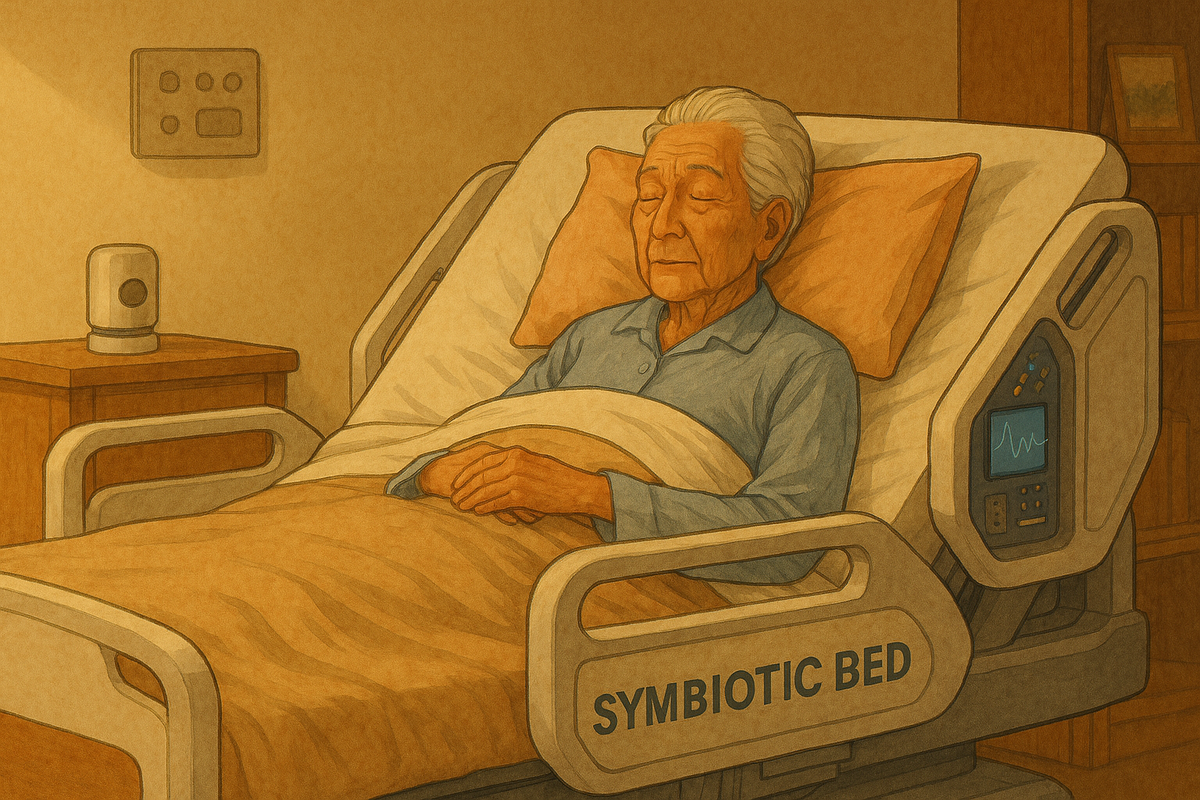
A New Vision: The Symbiotic Bed
Elderly individuals often spend long hours in bed. For many, the bed is where they sleep, eat, read, recover, and connect with others. The Symbiotic Bed reimagines this intimate space as a partner in care. Not a machine in the room — but the room itself, made intelligent.
Features:
- Automatic rotation to prevent bedsores
- Discreet toilet and hygiene module
- Feeding and hydration system
- Voice assistant for reading, video calls, music
- Health monitoring (pulse, temp, motion, hydration)
- Emotional support: calm voice, routines, reminders
Design Principles:
- Familiar, not futuristic: No humanoid parts, no blinking eyes
- Modularity: Sensor packs, software, and comfort elements can be upgraded
- Human-centered: Designed for physical comfort and emotional ease
This vision must go beyond beds and into the very buildings where older adults live. The truth is stark: very old individuals—those who no longer control their biological functions, whose cognitive capacities have weakened—should not be expected to live in homes originally built for the young and able-bodied. These spaces betray them. Doors require assistance. Stairs become insurmountable obstacles. “But there’s an elevator,” some might argue. Yet when that elevator breaks or is under inspection—a process that may take an entire day—the resident is trapped. Inside the apartment, high kitchen counters, heavy pots, or unreachable fridges render daily life impossible. The stove remains on. The bath is deep and dangerous. All this must be retrofitted at great expense—and still remains inadequate.
Worst of all, when that person dies—alone in their chair or bed—they may remain undiscovered for days or even weeks. This, particularly in Japan, is far too common. It is undignified.
We must abandon the romantic but misguided idea that housing for dependent elders should look like normal housing. That is fantasy. What we need are environments conceived from the start as intelligent systems. The kitchen must be a machine—tracking food, restocking autonomously, even monitoring the well-being of its resident. The bathroom must be a machine—providing hygiene for a person who cannot stand. No more irrational and exhausting tasks for staff—lifting, washing, transferring.
These are not luxuries. They are the bare minimum if we mean to honor the dignity of those at the end of life. For that, we younger people must confront a truth we would rather avoid: one day, we too will urinate and defecate in bed. The desire for dignity demands that we reject illusions and prepare environments that see aging for what it is—not who we once were, but who we will become.
Ethics at the Core
Technology in elder care must uphold human dignity. The Symbiotic Bed is designed not to replace nurses or family, but to support them. Key ethical pillars:
- Autonomy: It helps the elder do more for themselves
- Transparency: The AI must explain what it’s doing, and why
- Privacy: Data must be secure and used responsibly
- Emotional honesty: It may offer comfort, but never pretend to be human
Why Not Humanoids?
- Technically complex, with many moving parts
- Uncanny appearance can disturb rather than reassure
- High cost with limited real-world usefulness
- The bed is already part of life — no adjustment needed
A Day in Kanagawa: Yuki's Story
Yuki, 87, lives in a care home outside Yokohama. Her Symbiotic Bed adjusts her posture at night to prevent soreness. In the morning, it offers her favorite tea and reads poetry while she waits for her caregiver. Her granddaughter calls every Saturday via the bed’s video screen. Yuki smiles more now. Not because she is surrounded by robots, but because the technology in her life is quiet, kind, and useful.
Policy Lessons
Japan's experience reveals a central lesson: when technology is invisible and non-intrusive, it works best. Policymakers should prioritize:
- Support for modular assistive tech
- Interdisciplinary design teams (engineers, caregivers, ethicists)
- Strong data governance
- Pilot programs that measure emotional as well as physical outcomes
Final Thoughts
In elder care, the future need not look like science fiction. It can look like a good day in bed: warm, calm, responsive. The Symbiotic Bed is not a robot. It is a companion in stillness — a quiet partner in dignity.
Annotated Sources for the Curious Reader
- Japan Tests AIREC Robot for Elderly Care – Interesting Engineering: Introduces AIREC, a full-body humanoid robot tested for patient rolling and hygiene support. Promising, but not yet commercialized.
- Japan's Push to Automate Elder Care – MIT Technology Review: Overview of Japan's technological ambition in elder care and why humanoids like Robear face real-world limitations.
- Use of Sensors in Elderly Care – J-STAGE: A literature review outlining 11 application areas for sensors, including fall detection and emotional cue recognition.
- Priority Fields in Long-Term Care Policy – METI Japan: Japan's 2024 roadmap outlines expansion areas such as nutrition, dementia care, and standardization across care technologies.
- AIREC: An AI-Powered Robot – SilverEco: Summarizes pilot deployments of AIREC and their outcomes in Japanese facilities.
- Digital Reflection in Care – Frontiers in Digital Health: Explains how care data can be visualized to help staff adapt routines and improve safety.
- Digital Strategies for Dementia – World Economic Forum: Discusses community-based design and co-creation as ethical priorities in Japan's dementia care.
- Japan's Elderly Care Revolution – Medical Japan: Offers insights into challenges of cultural acceptance and emotional design in assistive technologies.
Essay by Richard P. Kindlman. Sources accessed and annotated November 2025.